The diabetes-mouth connection
- People with diabetes have a greater risk of developing dental problems like gum disease and infections. Having gum disease can also worsen complications from diabetes
- Your dentist can look for signs if you’re at risk for diabetes, or that your existing diabetes may not be well-controlled.
- Treating either gum disease or diabetes can lead to improvements in the other.
Research shows that diabetes and oral health can affect each other. This means if you have diabetes, you are at greater risk for developing dental problems like gum disease and infections. On the other hand, having gum disease can also worsen complications from diabetes by increasing blood sugar levels.
The good news is that treating either gum disease or diabetes can lead to improvements in the other!
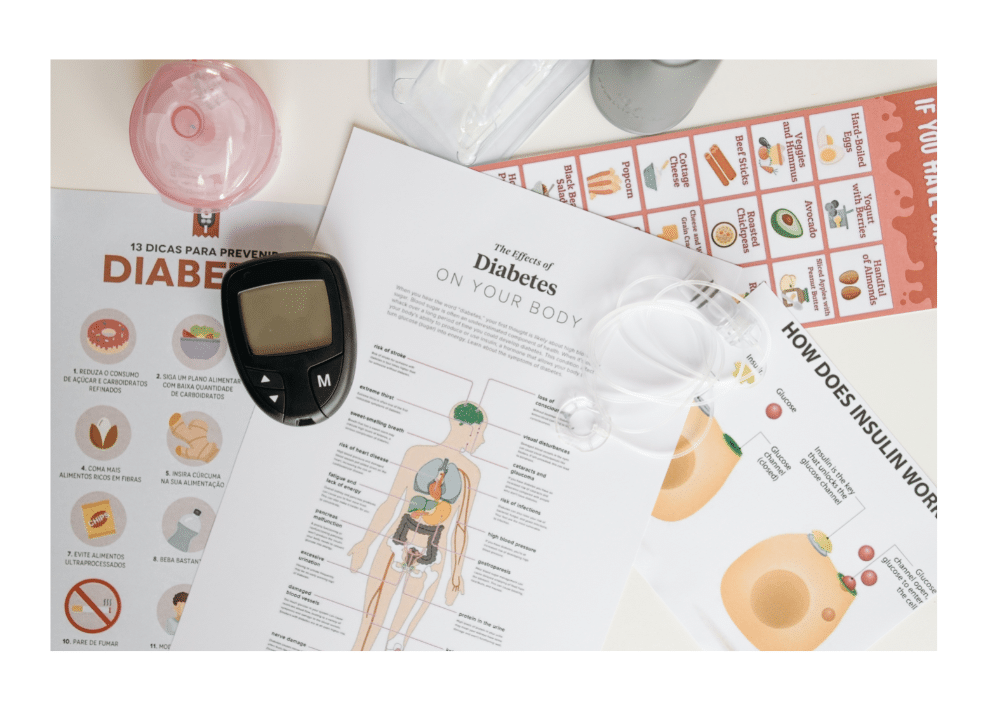
What is diabetes?
Diabetes is a medical condition in which the body does not produce or properly use insulin – a hormone needed to absorb sugar. As a result, the body cannot use sugars from food, which are the basic fuel for cells. Untreated diabetes can lead to heart disease, kidney disease, nerve damage and infections, and other serious complications.
Symptoms
Some of the symptoms of diabetes are:
- unusual thirst
- frequent urination
- extreme fatigue
- blurred vision
- frequent or recurring infections
- cuts and bruises that are slow to heal
- tingling or numbness in hands or feet
How can diabetes affect my mouth?
Too much glucose (sugar) in your blood from diabetes can cause pain, infection, and other problems in your mouth. This can affect your teeth, gums, jaw, and tissues such as your tongue, cheeks, and mouth.
Through an oral examination, your dentist will look for certain oral-health conditions that could signal a need for you to be tested for diabetes. The most common dental problems found in people with diabetes include:
- gum disease
- tooth decay
- dry mouth
- fungal infections
- lesions in the mouth
- loss of taste
- infection and delayed healing
How can my mouth affect my diabetes?
The relationship between serious gum disease and diabetes is two-way. Not only are people with diabetes more likely to get periodontal disease – chronic infection of the gums – but research also suggests that people with chronic, uncontrolled gum infections may be more likely to get diabetes.
People with diabetes are more likely to have periodontal disease because diabetics are more susceptible to contracting infections. Type II diabetics are 3 times more likely to develop gum disease (20 times more likely if they smoke!). Recent studies also confirm that the inflammation associated with periodontal disease also may increase insulin resistance, thereby aggravating glycemic control. It can become a vicious cycle.

Why people with diabetes are more prone to gum disease
Glucose is present in your saliva—the fluid in your mouth that makes it wet. When diabetes is not controlled, high glucose levels in your saliva help harmful bacteria grow. These bacteria combine with food to form a soft, sticky film called plaque. Plaque also comes from eating foods that contain sugars or starches. Some types of plaque cause tooth decay or cavities. Other types of plaque cause gum disease and bad breath.
If plaque is left untreated, it can lead to periodontal disease. This chronic, inflammatory disease can destroy your gums, all the tissues holding your teeth, and even your bones.
Periodontal disease is the most common dental disease affecting those living with diabetes, affecting nearly 22% of those diagnosed. Especially with increasing age, poor blood sugar control increases the risk for gum problems. In fact, people with diabetes are at a higher risk for gum problems because of poor blood sugar control. As with all infections, serious gum disease may cause blood sugar to rise. This makes diabetes harder to control because you are more susceptible to infections and are less able to fight the bacteria invading the gums.
Diabetes takes a toll on your entire body, but it can also increase your risk of dental disease and other symptoms that show up in your mouth. In fact, one in five cases of total tooth loss is linked to diabetes. The good news is you can take charge of your health today. Controlling your blood sugar, brushing, flossing and visiting your dentist regularly can go a long way to help decrease the likelihood of developing these diabetes-related mouth issues.

The problem with plaque
Plaque that is not removed hardens over time into tartar and collects above your gum line. Tartar makes it more difficult to brush and clean between your teeth. Your gums become red and swollen, and bleed easily—signs of unhealthy or inflamed gums, called gingivitis.
When gingivitis is not treated, it can advance to gum disease called periodontitis. In periodontitis, the gums pull away from the teeth and form spaces, called pockets, which slowly become infected. This infection can last a long time. Your body fights the bacteria as the plaque spreads and grows below the gum line. Both the bacteria and your body’s response to this infection start to break down the bone and the tissue that hold the teeth in place. If periodontitis is not treated, the gums, bones, and tissue that support the teeth are destroyed. Teeth may become loose and might need to be removed. If you have periodontitis, your dentist may send you to a periodontist, an expert in treating gum disease.
How your dentist can help
Because your dentist is an expert in oral health, they will know what to look for during your check-ups. If they find signs that you are at risk for diabetes, or that your existing diabetes is not well-controlled, they will refer you to your family doctor for follow-up treatment or testing.
At your next visit, be sure to tell your dentist:
- If you have been diagnosed with diabetes and if the diabetes is under control.
- If you take insulin and when your last usual dose of insulin was taken.
- If there has been any other change in your medical history.
- The names of all the herbal medicines, prescription and over-the-counter drugs you are taking.
Your best defense from diabetes-associated periodontal disease is a good home oral health care routine and regular check-up and cleanings.

How can I prepare for a visit to my dentist?
Plan ahead. Talk with your doctor and dentist before the visit about the best way to take care of your blood glucose during dental work.
You may be taking a diabetes medicine that can cause low blood glucose, also called hypoglycemia. If you take insulin or other diabetes medicines, take them and eat as usual before visiting the dentist. You may need to bring your diabetes medicines and your snacks or meal with you to the dentist’s office. You may need to postpone any non-emergency dental work if your blood glucose is not under control.
If you feel nervous about visiting the dentist, tell your dentist and the staff about your feelings. Your dentist can adapt the treatment to your needs. Don’t let your nerves stop you from having regular checkups. Waiting too long to take care of your mouth may make things worse.
How your dentist can help you fight diabetes
Regular dental visits are important. Research suggests that treating gum disease can help improve blood sugar control in patients living with diabetes, decreasing the progression of the disease. Practising good oral hygiene and having professional deep cleanings done by your hygienist can help to lower your HbA1c. (This is a lab test that shows your average level of blood sugar over the previous three months. It indicates how well you are controlling your diabetes.)
Your diabetes-dental health action plan
- Tell your dentist that you have diabetes
- Tell your dentist about any changes in your health or medicines
- Share the results of some of your diabetes blood tests, such as the A1C test or the fasting blood glucose test
- Keep your blood glucose numbers as close to your target as possible. Your doctor will help you set your target blood glucose numbers and teach you what to do if your numbers are too high or too low.
- Maintain a healthy diet and exercise regularly to help control your blood sugar. Good control of your glucose levels will also help your body fight any bacterial or fungal infections in your mouth and help relieve dry mouth caused by diabetes.
- If you wear any type of denture, keep it clean and take it out every night. Have your denture adjusted if it becomes loose or uncomfortable.
- Brush your teeth twice a day with a soft toothbrush and fluoride toothpaste
- Using small, circular motions, brush gently, angling the brush towards the gum line.
- Brush the front, back, and top of each tooth. Brush your tongue, too.
- Aim for brushing first thing in the morning, before going to bed, and after each meal and sugary or starchy snack.
- Use dental floss, following your hygienist and dentist’s instructions. Using a clean section of floss as you move from tooth to tooth, be sure to curve the floss around the base of each tooth and under the gums. Flossing helps prevent plaque from building up on your teeth.
- Sometimes a dental pick or special brush may be recommended to help you clean between your teeth. Your hygienist will recommend the tools that are right for you.
- Call the dentist right away if you have any symptoms of mouth problems.
- If your dentist tells you about a problem, take care of it right away.
- If you smoke, stop smoking.
Diabetes can cause gum disease to be more severe and take longer to heal.
Gum disease can make your blood glucose difficult to control.